What is obsessive-compulsive disorder (OCD)?
Obsessive-compulsive disorder, known widely as OCD, is a mental health disorder, in which someone has repeated unwanted thoughts, feelings or behaviour. It can be characterised by repeated intrusive thoughts or sensations (obsessions) and rituals (compulsions) aimed at reducing the distress they feel. Some sufferers of the disorder can experience both obsessions and compulsions.
Although most people have habits or repetitive thoughts sometimes, OCD is a severe disorder that can be incredibly distressing and debilitating. OCD may cause individuals to feel frequently tense, anxious, fearful, guilty, disgusted or depressed.
Often, they understand that their thoughts, feelings and actions do not make sense; however, they find they cannot stop. Sufferers usually feel better if they carry out their compulsive behaviour or ritual.
OCD can affect people of all ages and genders. Symptoms can start to show in childhood or teenage years but usually develops in adulthood.
Signs and symptoms of obsessive-compulsive disorder (OCD)
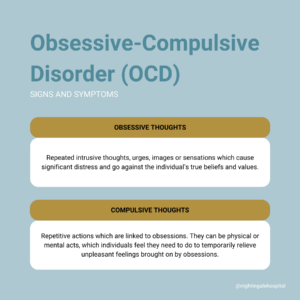
Most people with OCD will suffer from obsessive and/or compulsive thoughts.
Obsessions
Obsessions are unwanted, unpleasant and repeated thoughts, images, doubts or ruminations in your mind. You try not to think about them, but they won’t go away. They may wonder for hours whether you might have caused an accident or misfortune to someone, endlessly argue with themselves or bothered, in a way that other people are not if things are not in exactly the right order, not balanced or not in the right place.
Compulsions
Compulsions are mental acts or repetitive behaviour. Individuals with OCD experience obsessional thoughts like counting or saying a special word over and over again or avoidance by avoiding touching particular objects, going to certain places taking risks or accepting responsibility. They may have rituals such as washing hands frequently or repeatedly asking others to tell them that everything is alright.
There are a number of mental health problems linked to OCD that involve repetitive thoughts, feelings and urges. Examples of similar conditions include body dysmorphic disorder (BDD), compulsive skin picking (also known as CSP), trichotillomania, perinatal OCD and hoarding.
What causes obsessive-compulsive disorder (OCD)?
The main causes of obsessive-compulsive disorder (OCD) according to research, tend to be:
- Genetics
- Depression, anxiety or ‘tics’
- Trauma
- History of physical or sexual abuse as a child
Treatment for obsessive-compulsive disorder (OCD)
Nightingale Hospital offers a range of treatments for OCD. You may receive support as an outpatient or inpatient.
Therapy
There are two main types of cognitive behavioural therapy, known as CBT, that treat OCD.
- Exposure Response Prevention (ERP) is a way to stop compulsive behaviours and anxieties strengthening each other by gradually facing your fears and learning to prevent the usual compulsive behaviours.
- Cognitive Behavioural Therapy (CBT) is a goal-directed, systematic and problem-solving therapeutic approach that focuses on the way we think. It acts in order to help overcome and manage emotional difficulties.
Medication can also be effective in improving OCD symptoms. It can be used in combination with CBT to reduce obsessions and compulsions.
Specialist OCD and related disorders inpatient service at Nightingale Hospital
The OCD and related disorders unit at Nightingale Hospital is a 6-bedded inpatient service, dedicated to treating patients with OCD. It is a private and unique service, specialising in the intensive delivery of cognitive behaviour therapy (CBT). The unit is under the leadership of world-renowned expert, Professor David Veale.
An inpatient admission will usually be suggested if:
- Your symptoms are very severe, you cannot look after yourself properly or you have thoughts about suicide
- You have other serious mental health problems, such as an eating disorder, schizophrenia, psychosis or a severe depression
- Your OCD prevents you from getting to a clinic for treatment
Specialist OCD and related disorders day therapy programme at Nightingale Hospital
Our OCD and related disorders day therapy programme is dedicated to treating patients with obsessive-compulsive disorder (OCD) and OCD-related disorders in an outpatient setting.
The treatment programme has been developed in line with the National Institute for Health and Care Excellence (NICE) guidelines for OCD and BDD. The OCD treatment programme is focused on cognitive behavioural therapy (CBT) and the integration of self-directed exposure tasks, comprising of both group and individual sessions. The specialist multidisciplinary team is led by Kiren Kaulder, Lead therapist for OCD and related disorders and Sumitra Patel, Day Therapy Lead.
A day therapy programme may be suggested:
- To support patients transitioning from primary inpatient care
- For those who do not need inpatient care
Repetitive Transcranial Magnetic Stimulation (rTMS) for obsessive compulsive disorder (OCD)
Repetitive Transcranial Magnetic Stimulation (rTMS) is a non-invasive method of brain stimulation.
The basic principle of Repetitive Transcranial Magnetic Stimulation (rTMS) is to target short magnetic pulses over the scalp in specific brain regions that regulate mood.
rTMS is a medically safe treatment that has been evidenced to significantly decrease symptoms of depression and OCD.