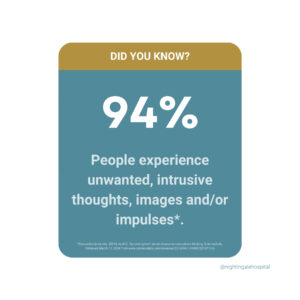
Intrusive or unwanted thoughts are a more common experience than most people realise. In fact, research has found that 94% of people experience unwanted, intrusive thoughts, images and/or impulses.
However, despite how common intrusive thoughts are, there is still a lot of misunderstanding around them. We sat down with Freddie, a former patient of the Nightingale Hospital OCD and related disorders unit, to talk about his experience with intrusive thoughts, what he has learnt about managing them and his encouragement for people who might be struggling.
Freddie’s experience with intrusive thoughts
“‘I am a monster’, ‘I don’t deserve to live’, ‘I’m a disgrace to my family’ and ‘I’m a freak’ – these were my beliefs and the way I viewed myself when I started to experience intrusive thoughts regularly. I felt like a monster, a creep and just a really bad person. I couldn’t live inside my head,” Freddie explained.
Intrusive thoughts are unwanted thoughts, images and/or impulses that are usually strange and disturbing. They might also be violent, sexual, or a recurring fear of doing something inappropriate or embarrassing. For example, thinking that you will push someone in front of a train is an intrusive thought.
Freddie explained that his fear about the intrusive thoughts he was experiencing was based on two things: one, that he was a bad person and two, that he would offend someone and people would think he is disgusting. “To try and reduce my fears, I turned to compulsions. They began with rhyming bad words or thoughts with neutral words and by doing so I would be reducing both fears. I began to hold my lips 24 hours of the day and set up a video camera to make sure, or check, that I wasn’t saying anything bad. My life was horrific, and it felt like constant torture. I felt desperate. I just wanted my life back.”
People with OCD may recognise that their thoughts, feelings, and actions are irrational, but they feel they often feel powerless to stop them. Engaging in their compulsions or habits usually provides temporary relief.
How common are intrusive thoughts?
“Intrusive thoughts are so, so normal – I can’t stress that enough. When we start reacting to them and believing that they somehow have any bearing on our personality, that’s when they don’t go away and just continuously play on our minds. If we didn’t experience intrusive thoughts, that’s what would make us not normal. Having intrusions is normal.”
One of the most common misconceptions about intrusive thoughts is that you unconsciously want to do the things that come into your mind. This is completely untrue. Freddie explains what he now understands about intrusive thoughts, “Experiencing paedophilic, sexual or racist thoughts can torment anyone. But for someone with OCD, the intrusions they are having are guaranteed to be the opposite of their values. That’s why when someone experiences them, they react to them, trying to get rid of them, as they do not fit in line with one’s core beliefs.”
Just as Freddie explained, we fight against intrusive thoughts because the thoughts feel at odds with who we are, and it is this effort used to fight the thoughts that make them stick and return.
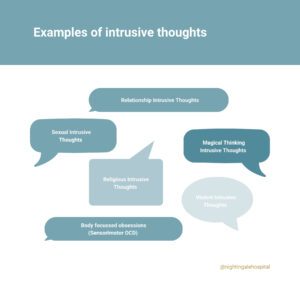
What are examples of intrusive thoughts?
While intrusive thoughts can encompass any imaginable topic, those frequently associated with OCD typically fall into several distinct categories.
- Relationship Intrusive Thoughts
- Sexual Intrusive Thoughts
- Magical Thinking Intrusive Thoughts
- Religious Intrusive Thoughts
- Violent Intrusive Thoughts
- Body focussed obsessions (Sensorimotor OCD)
At the one-year anniversary of the OCD and related disorders unit, we asked attendees to submit an intrusive thought they have had. We invited former patients, staff and other guests to submit an intrusive thought. These were some of the thoughts submitted:
- Jump onto the train tracks
- Kick my dog
- If I don’t repeat the mantra, I will fail
- Stabbing my mum with a kitchen knife
- Avoid the camera
- Having my throat cut
Can you stop intrusive thoughts?
Intrusive thoughts cannot be stopped directly – after all, they affect nearly everyone. However, there are ways you can manage them.
When asked about how Freddie manages his intrusive thoughts, he said, “Something that helped me is writing them down, putting posters up and sharing them with loved ones. Once you accept the thought, let it be there, let it float away, and almost become friends with it, the quicker you’ll get your life back. By accepting them, it does not mean you are those thoughts, it just means you accept that you are having a strange intrusive thought, and you are not going to react to it or let it control your life.”
Intrusive thoughts are very common and should be thought of as just a purely mental event; a ‘thought’ and nothing more.
Freddie’s encouragement to anyone struggling with intrusive thoughts
“If someone is out there and like me for a long time, believes that intrusive thoughts are unacceptable and abnormal, please allow me to share an analogy. We do not tell our heart to pump blood around our body, our breathing is automatic and so is the brain. We don’t ask the brain to allow us to have intrusions, it’s just part of biology. In the same way, intrusive thoughts are normal. After a lot of pain and work at Nightingale, I have gone from being too scared to eat in the canteen, to now taking the tube on my own, getting discharged and going to university. I am now living life, going travelling with friends and it is all down to the work I did, the things I learnt and the understanding I have from Nightingale.
You are not alone.
You are not your intrusions.
You are not a monster, OCD is.
Never be afraid to reach out. You can do it.”
For anyone struggling with intrusive thoughts or OCD, Freddie highly recommends Professor David Veale’s book, ‘Overcoming Obsessive Compulsive Disorder’.
Support is available
Nightingale Hospital offers a range of treatments for those experiencing intrusive thoughts or OCD. The OCD and related disorders unit at Nightingale Hospital is a 6-bedded inpatient service, dedicated to treating patients with OCD and related disorders. It is a private and unique service, specialising in the intensive delivery of Cognitive behavioural therapy (CBT). The unit is under the leadership of world-renowned expert, Professor David Veale.
We also offer an OCD Day therapy programme which is designed as a 2-day per week, 4-week day patient treatment programme to support patients transitioning from primary inpatient care or for those who do not need inpatient care. The treatment is delivered as a face-to-face programme at our location in Marylebone, London.
“We have developed an evidence-based treatment programme unlike any other, and we have seen incredible results. We have witnessed individuals whose lives were once overtaken by anxiety begin to reclaim their lives and find the hope and confidence to move forward. We have seen families who were once overwhelmed, find a sense of relief as they watched their loved ones make progress and regain their sense of self,” said Kiren Kaulder, the Lead therapist of the OCD and related disorders unit.
Related Conditions
Treatment approaches
- OCD and related disorders unit
- OCD day therapy programme
- Cognitive behavioural therapy (CBT)
- Prescription nasal spray for treatment-resistant depression
Relevant specialists
-

Professor David Veale
Lead consultant for OCD and related disorders at Nightingale Hospital









