Self-harm: What is it, types, signs, prevalence, causes, and treatment
What is self-harm?
Self-harm occurs when someone intentionally hurts themselves or injures their body without an intent to die. Self-harm may be linked to negative experiences that someone is currently experiencing, but it could also be in response to past experiences.
After self-harming, people may feel a short-term sense of release or control. This can make them more likely to depend on it and less able to stop, creating a cycle of harming themselves routinely. But it’s likely that difficult feelings will return soon after. This can include feelings of guilt or shame.
Individuals engaging in self-harm may feel as though the act is the only thing that can distract them from the emotional pain they are experiencing. While some people engage in self-harm infrequently, others do so repeatedly over time. It is important to recognise that self-harm is a symptom of underlying distress rather than attention-seeking behaviour.
Get support for self-harm
We understand that reaching out to someone you don’t know about what you’re experiencing can be a big step. Our team is here to offer a confidential conversation to discuss your concerns and how we can support you, through assessment and treatment. Complete the enquiry form below and our team will be in contact with you.
Why do people self-harm?
Each person’s reasons for self-harming and causes of their emotional distress will be different and often there is no single reason. It can be a combination of social and psychological factors as well as stressors that contribute to the development and maintenance of self-harm behaviours.
Some people have described self-harm to:
- Express something that is hard to put into words
- Turn invisible thoughts or feelings into something visible
- Change emotional pain into physical pain
- Reduce overwhelming feelings or thoughts
- Feel more in control
- Escape traumatic memories
- Have something in life that they can rely on
- Punish themselves for their feelings and experiences
- Stop feeling numb, disconnected or dissociated
- Create a reason to physically care for themselves
- Express suicidal feelings and thoughts without taking their own life
- Manage an underlying mental health condition
- Manage life changes
Content Warning
Some of the information below discusses self-harm and may be upsetting or triggering. If you’re feeling vulnerable or distressed, you might not want to read the information below.
There are details of where to find help at the bottom of this page.
Types of self-harm
Some common types of self-harm are:
- Cutting, scratching or piercing the skin with a sharp object, is one of the most common methods
- Burning the skin
- Over-eating or under-eating
- Self-hitting, punching, biting or head banging
- Repeatedly scratching the same area of the skin leading to skin damage
- Self-poisoning by consumption of harmful agents like poisons, household substances or medications
- Risk-taking behaviour like jumping from heights or in front of vehicles
- Alcohol and/or drug misuse
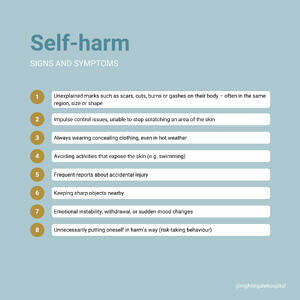
Signs of self-harm
Signs of self-harm can be subtle and often hidden. Here are a few signs that may suggest someone is hurting themselves:
- Unexplained marks such as scars, cuts, burns or gashes on their body – often in the same region, size or shape
- Impulse control issues, unable to stop scratching an area of the skin
- Always wearing concealing clothing, even in hot weather
- Avoiding activities that expose the skin (e.g. swimming)
- Frequent reports about accidental injury
- Keeping sharp objects nearby
- Emotional instability, withdrawal, or sudden mood changes
- Unnecessarily putting oneself in harm’s way (risk-taking behaviour)
Who is at risk?
Self-harm can affect anyone, regardless of age, gender, or background. However, certain factors increase the likelihood of engaging in self-harm:
- Mental health conditions such as depression, anxiety, borderline personality disorder (BPD), post-traumatic stress disorder (PTSD), and eating disorders
- History of trauma or abuse (physical, emotional, or sexual)
- Difficulties with emotional regulation
- Social isolation or bullying
- Low self-esteem
- Substance use
If you are struggling with self-harm, please know that you are not alone, and support is available.
Getting the right help can make a real difference in understanding and addressing the underlying causes.
If you are in crisis or feel unsafe, please go to your nearest A&E department or contact local emergency services for immediate support.
How common is self-harm in the UK?
- Approximately 1 in 14 people in the UK have self-harmed at some point in their lives.1
- UK data indicates that 60% of adults and 90% of young people aged 12-17 do not seek medical or psychological support after self-harming.2
- In England, it’s estimated that over 200,000 people seek hospital care every year due to self-harm, with most of these visits being for self-poisoning.3
- The prevalence of non-suicidal self-harm in England nearly tripled over a decade, increasing from 2.4% in 2000 to 6.4% in 2014.4

Treatment for self-harm
Self-harm is treatable, and professional support can help individuals develop healthier coping strategies. Effective treatment options include:
Therapy and Psychological Support
- Cognitive Behavioural Therapy (CBT): Helps individuals understand the thoughts and feelings that influence their behaviours. In the context of self-harm, CBT encourages patients to identify triggers and develop healthier coping mechanisms.
- Dialectical Behaviour Therapy (DBT): Designed for emotional dysregulation, DBT has proven effective for those exhibiting self-harming behaviours. It focuses on teaching skills such as mindfulness, distress tolerance, emotional regulation, and interpersonal effectiveness.
- Psychodynamic Therapy: Explores underlying emotional conflicts that contribute to self-harm.
Medication
- While there is no specific medication for self-harm, treating underlying conditions (such as depression or anxiety) with antidepressants or mood stabilizers may reduce the urge to self-injure.
Building Coping Strategies
- Engaging in alternative activities such as drawing, writing, or physical exercise can help manage emotions without self-harming.
- Developing distress tolerance skills, such as deep breathing or mindfulness, can provide healthier ways to cope with stress.
Social Support
- Connecting with trusted friends, family, or support groups can help reduce isolation and provide emotional support.
- Crisis helplines and online communities can offer immediate guidance.
We know the speaking to someone you don’t know about what you’re experiencing is a big step. We offer support for individuals struggling with self-harm and because we know the underlying reasons for self-harm differ for everyone, this support is tailored to your specific needs. Treatment and support options include outpatient, day patient, and inpatient care, depending on the support needed for the individual person.
Treatment at Nightingale begins with a thorough assessment with a consultant psychiatrist. From this assessment, a consultant psychiatrist will put together an individualised treatment plan and recommendation for you which may include medication, psychotherapy or CBT.
Useful resources
If you’re finding things difficult, you’re not alone—there are people who care and want to help. Below are some confidential support services available to you:
-
Samaritans: Call 116 123 or email jo@samaritans.org for free, confidential support 24/7.
-
MIND: Call 0300 123 3393 or text 86463 for mental health support, available weekdays from 9am to 6pm.
-
Shout: Text “SHOUT” to 85258 for 24/7 support via text.
-
HOPELINE247 (Papyrus): If you’re under 35 and struggling with thoughts of self-harm or suicide, call 0800 068 4141, text 88247, or email pat@papyrus-uk.org for free, confidential support 24/7.
-
Childline: If you’re under 19, call 0800 1111 for free, confidential support from trained counsellors.
-
NHS: Visit the NHS website for advice, coping strategies, and support resources related to self-harm.
Discovering that someone you care about is self-harming can be an emotional and overwhelming experience. It is natural to feel scared, confused, or even helpless.
However, your support can make a significant difference in their journey toward healing.
- MIND, Mental health facts and statistics
- Knipe, D., Padmanathan, P., Newton-Howes, G., et al. (2022) Suicide and self-harm. Lancet 399(10338), 1903-1916
- NICE, Self-harm is everyone’s business, NICE says in new draft guideline
- Major rise in non-suicidal self harm in England, study shows, doi:10.1136/bmj.l4058